The lifecycle of one of your patients starts long before they walk through your clinic’s doors – it starts the moment they land on your website or discover an article you’ve written when searching for a solution to their pain or problem. It extends well beyond your treatment of their initial problem and even beyond any maintenance appointments – they’re your customer for life, and you’ve built a lifelong trusting business relationship with them.
Within your patient’s life cycle comes a very important opportunity and preventable money leak: self-discharge from your treatment plan. Jarod Carte, a Doctor and the founder of the ‘Cash-Based Practice Bootcamp’, says “fortunes are made or lost by how well a practice minimises patient drop offs from the schedule. That is, minimising self-discharges by people that are not yet 100%”. And in the experience of medical and health clinics across a wide range of professions, this is very true. Here’s how self-discharge could be a major money leak for your clinic, the impact it’s having not only for you but your patients too, and how to help plug that money leak to boost your revenue and your treatment outcomes.
Self Discharge: The Impact On Clinics And Patients
Self-discharge is a big issue for all practices, and we’ve all experienced it – a patient whose pain reduces from a 8/10 on the VAS to a 3/10 does feel significantly better, and therefore may decide that they’ve gotten the most out of your services and that the rest of the pain will naturally take care of itself and reduce over time.
Identifying money leaks throughout the patient lifecycle isn’t just important for a clinic’s revenue. It is equally important for your patient’s health and long-term well-being. When patients stay committed to their treatment plan throughout the entire lifecycle, you are able best support them getting the most out of their recovery and health, while also building on a fantastic relationship that can lead to raving word-of-mouth referrals and build on your reputation as a clinic.
Practising self-autonomy through self-discharge against medical advice is regularly observed and studied across a range of services, whether that’s after surgery or simple antibiotic infection care, and consistently shows poorer patient outcomes and health-compromising behaviours. So how can practitioners continue to respect patients and their autonomy while reducing the prevalence of self-discharge?
The Information On Your Website And Your Marketing Avenues
Addressing self-discharge doesn’t start in your face-to-face appointment, but before this, in the information they read online on your website, or the welcome emails they are sent from you. Many clinics and marketing agencies choose to use the sales psychology that people want results instantly, and so purposefully create this impression – that the treatment process is going to be simple, quick or easy, even if they never use that wording.
This approach means that by the time your patient is meeting with you for the first time, they already have this quick and easy expectation. And if this is not addressed and then their expectations (even if unfounded) do not align with the true course of treatment and the rate of their progress, they may feel like ‘their treatment is not working’ (relative to their beliefs on the speed it should be working). They may think ‘the treatment has worked as much as expected, I can stop now’ based on not realising that with your help, they can get to 0/10, as well as set themselves up for future recurrence prevention.
The First Appointment
The first appointment is an important start to managing their expectations when it comes to their treatment. When discussing their treatment plan, it’s important to set very clear timeline expectations, including a realistic treatment time frame for them based on their unique factors and circumstances, and what the upper limit for treatment in general is – showing that in some cases it may take longer and that can be expected. Assure them that if it takes longer, this does not mean they are not getting results, it is simply the rate at which their body is responding in their specific circumstances.
Ensure to give them a clear vision of what the end goal looks like for this initial treatment period. Does it look like getting them to a place where they are strong and fit and pain-free to run that marathon? Is it getting their pain levels to 0? Is it something else? Clear up any confusion about what it is exactly that you are working to help them achieve, so they’ll consciously know they are stopping treatment too early when considering self-discharge.
If your care includes the potential maintenance appointments in the future, discuss these early and explain under what circumstances they may be necessary, and what tangible benefits they will bring to your patients.
During Each Treatment Visit
During each treatment visit, depending on how your services work, start with monitoring your patients progress and discussing the changes since the last visit. This helps affirm that your treatment plan is working and is important to stick to. If there has been a setback and results haven’t progressed as expected, take the time to explore why. Did their heel pain not improve because they spent the weekend in high heels which caused more damage? Did they try going for a run and their knee pain flared up? Find the answer and explain it to them.
Next, continue to remind them of where they’re going and the journey they’re on. If they’ve noticed significant progress, like a 30% pain reduction since the last appointment, they may think ‘I won’t have too many sessions left until I’m pain-free’ without realising that perhaps the last part of the program is the hardest, and then after that you need to focus on rebuilding strength, flexibility and mobility to set the patient up for success and help prevent pain recurrence. It may not feel the most comfortable to talk about and bring up, but you’re setting clear expectations and ensuring your patient doesn’t get the wrong idea based on either assumptions or experiences they hear from friends who were “fixed in two sessions”.
Be Transparent About Cost Expectations From Day One
Again, some practitioners do find it uncomfortable to discuss money and treatment costs, but we recommend being transparent about the number of sessions required and the treatment costs (which means your patients do run the figures in their mind) because this way you are more likely to onboard patients that are more likely to see the entire treatment cycle through with you. This is more important now than even given that many clinics are short-staffed and have limited openings for new patients. You want the right patient.
Remember Your Reputation
Remember that incorporating these principles of clarity and transparency throughout each appointment has an impact on your reputation, too. Having patients self-discharge when they’re not fully better can lead to feedback to others and referral sources that don’t give the complete picture of what you can offer and therefore may deter future patients.
What If They Can’t Afford The Treatment Cost?
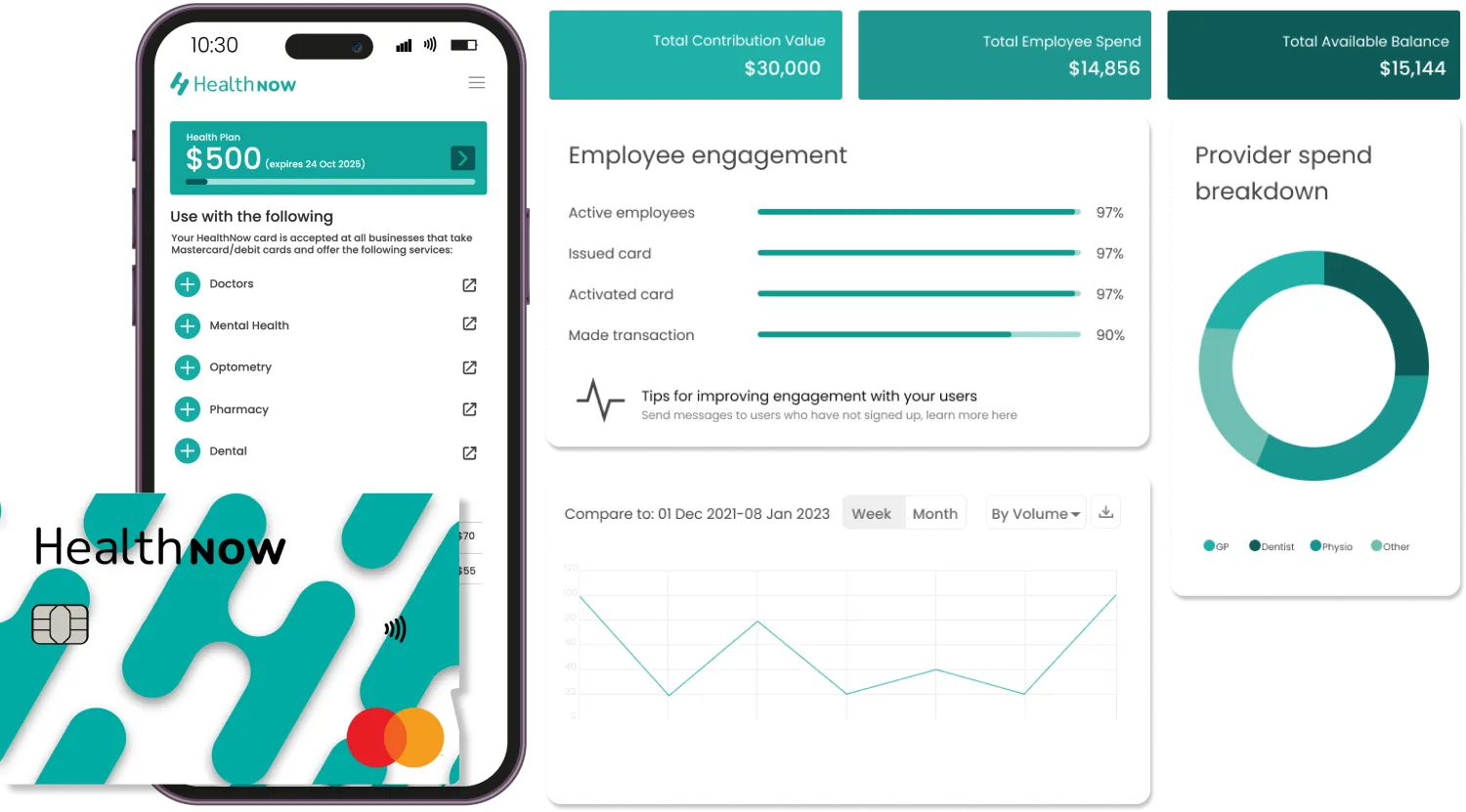
Money is undoubtedly a big factor in choosing to continue care, especially if notable results have been attained with the initial treatment period. One way New Zealand clinics are overcoming this challenge is by offering the world’s first health-focused Buy Now Pay Later (BNPL) platform called HealthNow as a payment option.
HealthNow lets patients spread the cost of your appointments, paying only a fraction of the total cost out of pocket on the day, while your clinic gets paid in full on the same day by HealthNow. Your patients can spread the cost over up to twelve weeks with no fees or interest.
Unlike other BNPL services, HealthNow meets a higher level of regulatory compliance to ensure that it operates with social responsibility. It is accessed via an app on patients’ smartphones, and is paired with a payment device at your reception that is provided to you by HealthNow.
HealthNow also has a specifically-designed health wallet that helps patients put away money safely to cover the costs of any medical or health-related appointments, services and products while accepting employer aid payment contributions – all of which can be used for your services for themselves or their family members.
Stop Money Leaks With HealthNow
There is no cost to sign up or integrate with HealthNow, and all training and support are completely free with no ongoing subscription or monthly charges. HealthNow also offers a free trial period so you can ensure it’s easy and simple to use, and right for your team.