In early March 2023, six more ambulances were turned away from Auckland Hospital due to the facility having an overcrowded emergency room. While this may seem like a one-off, the last few years has seen continuous reports from hospitals around the country – from repeated overcrowding that in some cases has led to some tragic consequences, to the high demands leading to hospital staff feeling psychologically and physically exhausted. While this is part of a much wider issue in NZ, one factor is the poor access to GPs and other emergency and urgent care facilities, at least in significant part attributed to the cost of attending these services.
The average price to see a doctor for an adult in Auckland is approximately $60. While a community services card reduces these fees to $18.50, these cards are issued to lower-income families and individuals, meaning that they already have limited funds to begin with in a climate where food prices, interest rates and the overall cost of living feels like it’s skyrocketing.
The Problem With Emergency Departments As A Free Solution
 With around one million visits annually by New Zealanders to public hospital emergency departments, while the cost-saving factor is a big drawcard, there are also several downsides. When any person attends the hospital emergency department, they are first triaged by a nurse to assess their level of need, and unless this is classified high enough to be a genuinely urgent medical need, you’ll be in for a very long wait – with one-third of patients in one DHB waiting for over six hours.
With around one million visits annually by New Zealanders to public hospital emergency departments, while the cost-saving factor is a big drawcard, there are also several downsides. When any person attends the hospital emergency department, they are first triaged by a nurse to assess their level of need, and unless this is classified high enough to be a genuinely urgent medical need, you’ll be in for a very long wait – with one-third of patients in one DHB waiting for over six hours.
The length of your waiting time will also be heavily influenced by the number of people in the ED (which rises notably over the winter months with various illnesses going around), and the queue times for diagnostic equipment given the limited equipment numbers and limited staff available to operate them at certain hours. Unfortunately, if someone comes into the ED after you that is classed as a higher priority based on their symptoms and condition, they will be seen first.
Unfortunately, it’s not just a long wait that you may be in store for. When emergency care is delayed, depending on the condition and symptoms, there can be notable health consequences. Research from Canada that looked at long waiting times as a result of overcrowded EDs showed that there was an increase in the risk of death and hospital readmission for those that were discharged. Other reports back these findings, showing an increased risk of the health of patients significantly deteriorating due to not getting the right treatment in time and an increased risk of adverse events. This may be connected to increased stress on staff, poorer adherence to protocols and clinical errors when there is overcrowding.
The potential for patients’ frustration, anxiety and stress to grow with the hours is also a concern, with those that wait long hours into the night having further potential impacts on their sleep and energy levels, concentration, mental clarity and work performance the following day.
What’s A Better Option – And How Can Alternative Urgent Care Be More Affordable?
 Thankfully, in today’s digital climate, there are several ways for kiwis to get access to their GP and urgent care facilities regardless of how much money is currently available in their bank account, helping them save time, frustration with waiting, and reduce the risk of poorer health outcomes from prolonged waiting periods – and the risk of errors and other consequences related to hospital overcrowding.
Thankfully, in today’s digital climate, there are several ways for kiwis to get access to their GP and urgent care facilities regardless of how much money is currently available in their bank account, helping them save time, frustration with waiting, and reduce the risk of poorer health outcomes from prolonged waiting periods – and the risk of errors and other consequences related to hospital overcrowding.
Employer aid payments
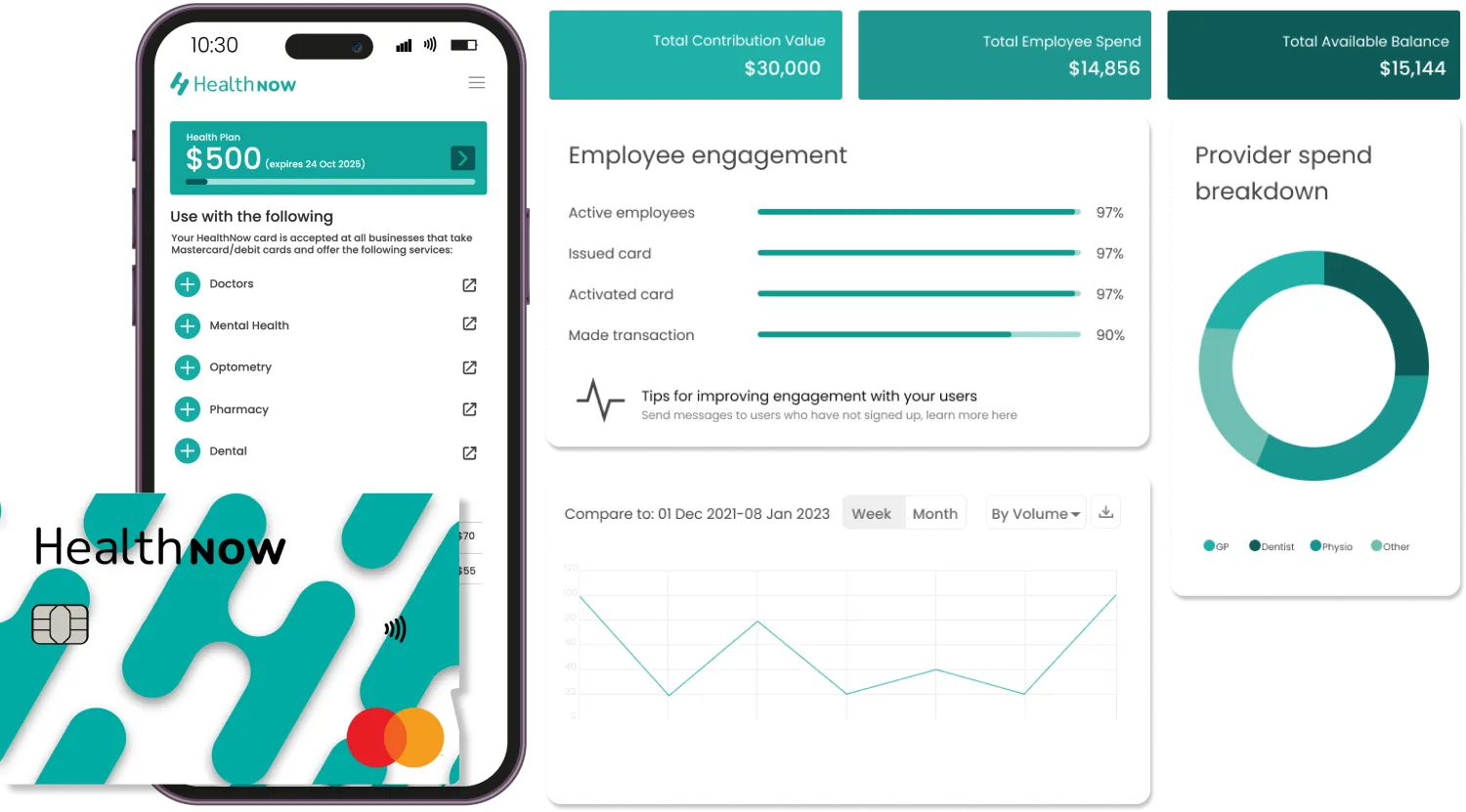
The first is through NZ businesses offering employer aid payments in place of traditional private health insurance with all of its limitations, restrictions, exclusions and stand-down periods. Specifically, funds are transferred into a dedicated digital health wallet such as that offered by HealthNow, which is then able to be used on any health and medical service and product – from doctors visits to pharmacy prescription costs.
Employers get the assurance that these funds are only able to be accessed and withdrawn at registered HealthNow medical providers, so are only being used towards bettering the health of their team – and helping them return to work faster in full health.
Health savers wallet
Another function of a digital health savers wallet is for self-insurance for those that want to periodically transfer money to be set aside to be used solely on health and medical expenses for themselves or their families. This is done entirely at the discretion of each person and family, meaning they are only ever contributing within their means. As there are no fees to health consumers to use the service at all, you retain all your money in full – alongside the $10 bonus you gain from HealthNow by joining their platform.
Buy now pay later
You can also access the care you need, when you need it, by opting to use HealthNow’s buy now pay later feature. Again, this is free to use for health consumers on a normal basis as long as you stay within their terms and conditions, and you’re able to spread the cost of your appointment over up to 12 weeks, at your discretion based on your financial circumstances at that moment in time. This allows you to access the care you need at a fraction of the cost on the day, while your health provider gets paid in full, making it a win-win.
Don’t Spend Hours Waiting For Health Access
Get the care you need, when you need it. Start by registering for HealthNow – it is free and easy. To start using HealthNow, download the app. You can also check out HealthNow’s full benefits and features, and see how it can make a big change in your family’s health.